This is an archived article that was published on sltrib.com in 2012, and information in the article may be outdated. It is provided only for personal research purposes and may not be reprinted.
An independent group of radiation oncologists affiliated with hospitals throughout Utah is hyping the arrival of "the world's most advanced radiation therapy."
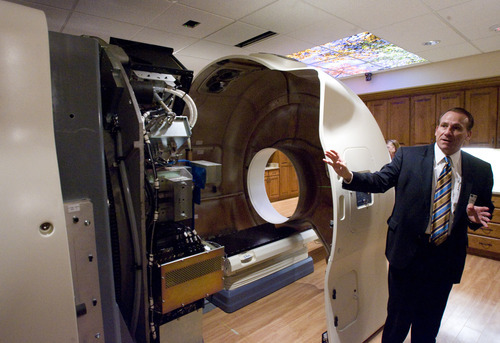
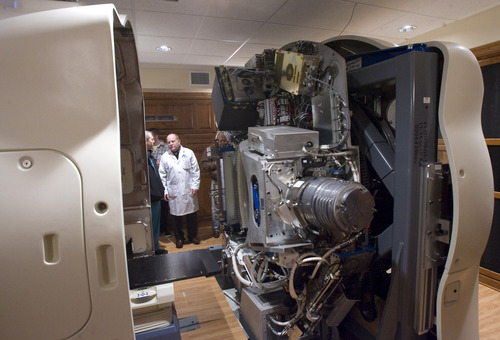
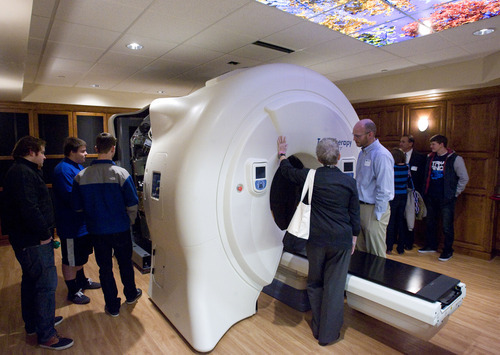
Residents of Davis, Washington — and now Salt Lake — counties have ready access to Accuray Inc.'s TomoTherapy Hi-Art Treatment System, says a news announcement by physicians at Gamma West Cancer Services. The technology, showcased in full-page newspaper ads and at a Friday open house at St. Mark's Hospital, takes 360-degree CT scans of patients, allowing radiologists to better spot tumors, pinpoint therapy and minimize damage to healthy tissue.
Experts agree image-guided radiation therapy is fast becoming the standard of care, especially for hard-to-reach tumors. But it isn't new technology, nor is it new to the Salt Lake area. And whether the TomoTherapy brand is "a step above" other systems, as described by Gamma West's founder and chief medical officer, John K. Hayes, is open for debate.
Image-guided therapy has existed since the mid-1990s under various brand names, said Bill Salter, radiation oncology director at the University of Utah's Huntsman Cancer Institute.
The goal of radiation oncology is to deliver focused doses of radiation, but tumors move as patients move and breathe, Salter said. "Image-guided radiation allows you to take pictures of tumors right before we treat to make sure we hit the tumor."
TomoTherapy units surfaced after the turn of the century. "I commissioned and installed one of these units in 2004 when I was at the University of Texas' Health Sciences Center," said Salter.
"This is very capable technology," he said. "There are lots of capable technologies."
Salter said newer systems, however, are better able to image soft tissues and map tumors.
"Think about the prostate, which moves around not just daily, but minute to minute," he said. "We have a system called Calypso where we implant GPS markers in the prostate to track its movement before and during treatment."
Gamma West radiation oncologist Rob Harris said these higher-voltage technologies expose patients to more radiation and can't be used on a daily basis. What's more, he said, TomoTherapy is more integrated, reliable and safer than other platforms.
The trick for patients, of course, is finding which treatments, if any, are right for them — a decision complicated by the soaring cost of cancer care in America.
From 1990 to 2008, spending on cancer grew to $90 billion from $27 billion, according to a 2009 study in the Journal of the American Medical Association. Authors tied the increase to new drugs, robotic surgeries, radiation techniques and an aging population.
The rise of high-tech medicine has coincided with a decrease in death rates from cancer. But scientists differ on whether it's directly responsible for prolonging lives.
"We are very medicalized in this country. We think that every predicament in life is a medical predicament and there's some miraculous solution," said Nortin Hadler, an immunologist and microbiologist at the University of North Carolina, Chapel Hill and author of Rethinking Aging and Worried Sick.
But about 80 percent of our increase in longevity is tied to our socioeconomic status — "something about the way we live together, whether that's job security or education levels," Hadler said.
Biomedical advances, on the other hand, are responsible for about 20 percent, which Hadler says he's proud of. But he rails against the overtreatment of patients by an industry that he says has "lost its moral compass."
Forget cost, he says. The question on every patient's mind should be, will this treatment work? "I don't care if they have the latest proton thing out of science fiction or if my insurance company will cover it or how well they market it. I care how much it will help my patient who is ill."
Just because you have high cholesterol, for example, doesn't mean you should take a statin, he said. "Cholesterol doesn't make you sick. It's a risk factor for heart disease. But studies show, in people who have never had a heart attack, the pill doesn't save lives."
Martin Murphy begs to differ, at least on the subject of image-guided radiation.
An engineer and physicist in the radiology department at Virginia Commonwealth University, Murphy has researched optimal radiation dosing using these machines. The technology for delivering radiation hasn't been around long enough to prove it saves lives, he said.
But the benefits of radiation therapy are clear, and data show today's high-tech delivery methods help doctors better control cancers with fewer side effects, Murphy said.
Lung cancer used to be a death sentence. But in the past five years, technologies like this have made local control of some lung cancers possible, he added.
Balancing the need for treatment with the risk of extra radiation exposure during imaging is technically tricky, said Murphy. "We're continually refining the treatment process. But these are not just expensive toys for physicians to play with. They work."
kstewart@sltrib.comTwitter: @kirstendstewart —
Evaluating care
The Cochrane Collaboration is a group of international scientists who investigate the upsides and downsides of all manner of medical interventions by reviewing the best available scientific literature. Their findings are open to the public at • cochrane.org/cochrane-reviews.