This is an archived article that was published on sltrib.com in 2012, and information in the article may be outdated. It is provided only for personal research purposes and may not be reprinted.
Advice to local doctors from the chief radiologist at one of the nation's leading medical schools: Mammography remains the most effective and affordable tool for detecting breast cancer and, for women with average risk of developing the disease, annual screening should begin at age 40.
That's contrary to advice from the U.S. Preventive Services Task Force, which two years ago took the controversial stand that women with no family history of the disease do not need to begin screening for breast cancer until age 50 and then should be tested every two years until age 74. It said there was insufficient evidence to show any benefit to continued testing after that age.
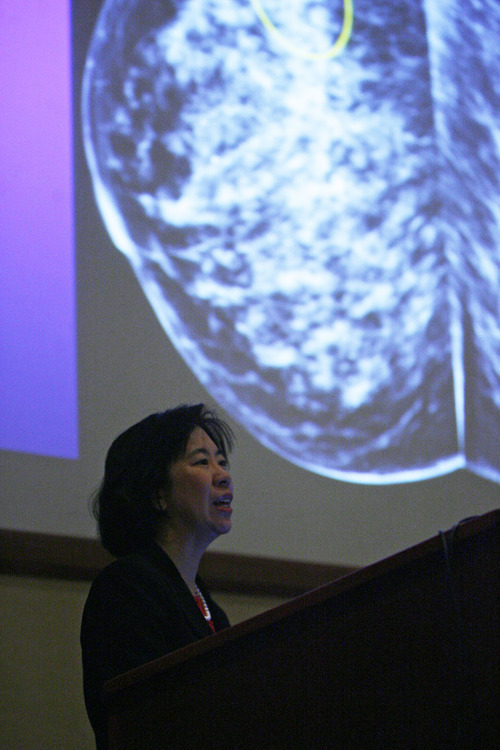
But Bonnie Joe, head of breast imaging at the University of California, San Francisco, said 70 to 80 percent of breast cancer diagnoses are in women with no family history or identifiable risk of the disease. Joe also said benefits of screening earlier and more often outweigh the "harms" — radiation exposure, pain caused by compression, testing anxiety, false results and over diagnosis — that the task force said led to its recommendations.
Joe said a typical mammography screening is equivalent to two months exposure to normal background radiation and is estimated to increase the lifetime risk of breast cancer from 1.3 to 1.7 cases in 100,000 women at age 40.
"So it's small, bottom line," Joe said. Also, "screening anxiety is not equal to death from breast cancer," she added.
Joe spoke Saturday at the 2012 Cowan Cancer Symposium at LDS Hospital, which this year focused on aspects of diagnosing and treating breast cancer. Sponsored by Intermountain Healthcare, the symposium provides continuing education for physicians. Breast cancer is the second leading cause of cancer death among women nationally, affecting one in eight during their lifetime. In Utah, it is the top cancer-related cause of death among women.
Joe reviewed the use of mammography, magnetic resonance imaging (MRI) and ultrasound to detect breast cancer. The effectiveness of mammography has long been established, she said. An organized mammography screening program in seven Swedish countries, covering 33 percent of the population, found breast cancer deaths were reduced 44 percent among women screened. A 2010 Swedish study, comparing counties in which screenings started at either age 40 or age 50, found a 29 percent decrease in breast cancer deaths among women ages 40 to 49.
She also cited a 2011 journal article that estimated 100,000 lives would be saved if all women currently ages 30 to 39 began annual screenings at age 40 — something the American Cancer Society continues to recommend.
Before age 40, only certain groups of women at high risk of developing breast cancer should receive routine mammogram screenings, Joe said.
If mammography is used with MRI, Joe said, the ability to detect the disease is even greater, especially among women at higher risk of breast cancer. According to one analysis, eight additional cancers were detected among 463 high-risk women who had an MRI following a mammogram.
The American Cancer Society recommends combined mammogram and MRI screenings for women with a family history, genetic tendency and certain other factors.
At UCSF, staff stagger mammogram and MRI screenings, alternating between the two every six months for high-risk patients, Joe said.
Twitter: @Brooke4Trib Proposed resolution urges Utah women to get annual screenings
An estimated 400 Utah women who have breast cancer will die this year— in part because they were diagnosed with the disease after it had already progressed to a late stage, according to a resolution proposed by a Utah lawmaker.
That's more than enough reason to urge women to get annual mammograms beginning at age 40, according to Sen. Karen Mayne, D-West Valley City.
On Monday, the Senate health committee will consider Mayne's resolution, SCR4, which emphasizes the importance of breast cancer screenings and encourages private health insurers to cover such tests at no or low co-payments. It also asks that public health programs provide screenings for uninsured women who cannot afford the tests.
Breast cancer is the leading cause of cancer-related deaths among women in Utah, the resolution states, yet the screening rates in the state are regularly at the bottom or among the lowest in the nation. It says many women skip screenings because of cost.
In 2012, an estimated 1,400 women will be diagnosed with the disease and nearly 40 percent will be at late stages. According to Mayne's resolution, treatment costs are estimated to be 1,000 times higher than if the disease had been caught earlier.