Al Hartmann | The Salt Lake Tribune
Hundreds of people rally at the Utah State Capitol Rotunda on Thursday, February 20 to supp
Al Hartmann | The Salt Lake Tribune
Hundreds of people rally at the Utah State Capitol Rotunda on Thursday, February 20 to supp
Al Hartmann | The Salt Lake Tribune
Hundreds of people rally at the Utah State Capitol Rotunda on Thursday, February 20 to supp
Al Hartmann | The Salt Lake Tribune
Hundreds of people rally at the Utah State Capitol Rotunda on Thursday, February 20 to supp
Al Hartmann | The Salt Lake Tribune
Hundreds of people rally at the Utah State Capitol Rotunda on Thursday, February 20 to supp
Al Hartmann | The Salt Lake Tribune
Hundreds of people rally at the Utah State Capitol Rotunda on Thursday, February 20 to supp
Al Hartmann | The Salt Lake Tribune
Hundreds of people rally at the Utah State Capitol Rotunda on Thursday, February 20 to supp
Al Hartmann | The Salt Lake Tribune
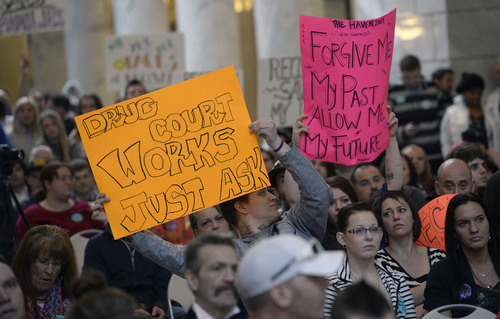
Hundreds of people rally at the Utah State Capitol Rotunda on Thursday, February 20 to support Medicaid expansion in Utah. If the state doesn't expand Medicaid by accepting federal funding, 58,000 low-income Utahns will fall into a "coverage gap" - receiving neither Medicaid coverage nor a tax subsidy to help purchase their own insurance.
Al Hartmann | The Salt Lake Tribune
Hundreds of people rally at the Utah State Capitol Rotunda on Thursday, February 20 to support Medicaid expansion in Utah. If the state doesn't expand Medicaid by accepting federal funding, 58,000 low-income Utahns will fall into a "coverage gap" - receiving neither Medicaid coverage nor a tax subsidy to help purchase their own insurance.
Al Hartmann | The Salt Lake Tribune
Hundreds of people rally at the Utah State Capitol Rotunda on Thursday, February 20 to support Medicaid expansion in Utah. If the state doesn't expand Medicaid by accepting federal funding, 58,000 low-income Utahns will fall into a "coverage gap" - receiving neither Medicaid coverage nor a tax subsidy to help purchase their own insurance.
Al Hartmann | The Salt Lake Tribune
Hundreds of people rally at the Utah State Capitol Rotunda on Thursday, February 20 to support Medicaid expansion in Utah. If the state doesn't expand Medicaid by accepting federal funding, 58,000 low-income Utahns will fall into a "coverage gap" - receiving neither Medicaid coverage nor a tax subsidy to help purchase their own insurance.
Al Hartmann | The Salt Lake Tribune
Hundreds of people rally at the Utah State Capitol Rotunda on Thursday, February 20 to support Medicaid expansion in Utah. If the state doesn't expand Medicaid by accepting federal funding, 58,000 low-income Utahns will fall into a "coverage gap" - receiving neither Medicaid coverage nor a tax subsidy to help purchase their own insurance.
Al Hartmann | The Salt Lake Tribune
Hundreds of people rally at the Utah State Capitol Rotunda on Thursday, February 20 to support Medicaid expansion in Utah. If the state doesn't expand Medicaid by accepting federal funding, 58,000 low-income Utahns will fall into a "coverage gap" - receiving neither Medicaid coverage nor a tax subsidy to help purchase their own insurance.
Al Hartmann | The Salt Lake Tribune
Hundreds of people rally at the Utah State Capitol Rotunda on Thursday, February 20 to support Medicaid expansion in Utah. If the state doesn't expand Medicaid by accepting federal funding, 58,000 low-income Utahns will fall into a "coverage gap" - receiving neither Medicaid coverage nor a tax subsidy to help purchase their own insurance.